As an Amazon Associate, Modded gets commissions for purchases made through links in this post.
You’ve just finished that plate of pasta or sandwich and there it is again – that oh-so-familiar discomfort. The bloating, brain fog, and accompanying digestive distress that periodically send you to the bathroom make you wonder why you have bad reactions after certain meals. If this sounds familiar, you might be dealing with carbohydrate intolerance. While it’s not the same as a full-blown food allergy, it can still make life uncomfortable.
What Is Carbohydrate Intolerance?
Do carbs make you gassy? Or have you ever wondered why some people can eat any amount of lasagna, bread and sugary treats without issues while others experience digestive distress, fatigue or mood swings? This could be due to carbohydrate intolerance, which occurs when the body struggles to break down certain sugars for energy in the small intestines. The undigested carbs move to the colon, where they trigger a reaction that results in abdominal pain, bloating, gas and watery diarrhea. People who are intolerant to carbs notice a craving for sugary treats, even after eating, because their bodies break down a few carbohydrates for energy.
This condition develops over time due to poor dietary habits, chronic stress or even antibiotic use that disrupts gut flora. Carbohydrate intolerance differs from celiac disease or food allergies, as it typically results in digestive discomfort rather than an immune response. However, if left unchecked, it can contribute to chronic inflammation, weight gain and an increased risk of metabolic disorders like type 2 diabetes.
Carbohydrate intolerance is more common than you think. Unfortunately, many people don’t even realize they have it until symptoms persist. Catching the problem early can help you make dietary adjustments before the condition severely impacts your quality of life.

Types of Carbohydrate Intolerance
Carbohydrate intolerance presents in several ways, each caused by different underlying factors. Understanding which type affects you can help you make the right dietary adjustments. They include:
- Lactose intolerance: The most prevalent form. Caused by a lack of the lactase enzyme needed to digest milk sugar, resulting in digestive discomfort after consuming dairy products. Symptoms typically include bloating, gas, stomach cramps and diarrhea.
- Fructose malabsorption: This occurs when the body has difficulty absorbing fructose. People with this intolerance experience digestive issues when consuming fruits, certain vegetables and processed foods containing high fructose levels.
- Sucrose intolerance: Results from a lack of enzymes needed to digest sucrose — table sugar. It leads to diarrhea, gas and stomach pain after consuming sugary foods.
- Congenital Sucrase-Isomaltase Deficiency (CSID): A genetic disorder present from birth that prevents the production of enzymes necessary for digesting sucrose and complex carbohydrates. This rare condition demands comprehensive dietary intervention and medical supervision.
- FODMAP sensitivity: A broader carbohydrate intolerance characterized by difficulty digesting Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols (FODMAPs) — short-chain sugars and fibers found in foods like onions, garlic, wheat and legumes. This condition is often linked to irritable bowel syndrome (IBS).
- Glucose-galactose malabsorption – A rare genetic disorder in which the body cannot properly digest glucose and galactose, symptomized by severe diarrhea and dehydration.
Each type of carbohydrate malabsorption presents unique challenges and requires tailored dietary strategies to manage symptoms effectively.
Why Does It Happen?
Factors contributing to carbohydrate intolerance include:
- Enzyme deficiencies.
- Gut bacteria imbalances.
- Metabolic conditions like insulin resistance.
- Genetic predispositions.
In some cases, the body’s inability to break down complex carbohydrates leads to excessive fermentation in the gut, causing bloating and discomfort.
Stress and lack of sleep can also exacerbate symptoms, making carbohydrate digestion even more complex. Addressing lifestyle factors alongside dietary changes can significantly improve tolerance over time. How old you are can also play a role, as some people become less efficient at digesting carbohydrates as they age.
Common Symptoms of Carbohydrate Malabsorption
Your body has ways of telling you when something’s not right. Most people with food intolerance symptoms chart a combination of immediate and delayed reactions. Immediate symptoms typically occur within minutes of eating and include:
- Bloating and excessive gas.
- Stomach pain or cramping.
- Diarrhea or loose stools.
- Unusual fatigue after meals.
- Increased sugar cravings.
Delayed reactions can be more subtle, emerging several hours to days after consuming trigger foods. These might include brain fog, unexpected weight gain, mood swings and unexplained joint pain or inflammation. Some people also experience headaches due to fluctuating blood sugar levels.
Other long-term issues related to carbohydrate intolerance can include insulin resistance, which can lead to type 2 diabetes, non-alcoholic fatty liver disease and even cardiovascular problems. If left unmanaged, chronic high blood sugar and inflammation may increase the risk of developing these health conditions.
These symptoms can sometimes be mistaken for disorders like food allergies or irritable bowel syndrome, so it’s best to monitor food reactions closely to rule out conditions that present as carbohydrate indigestion.
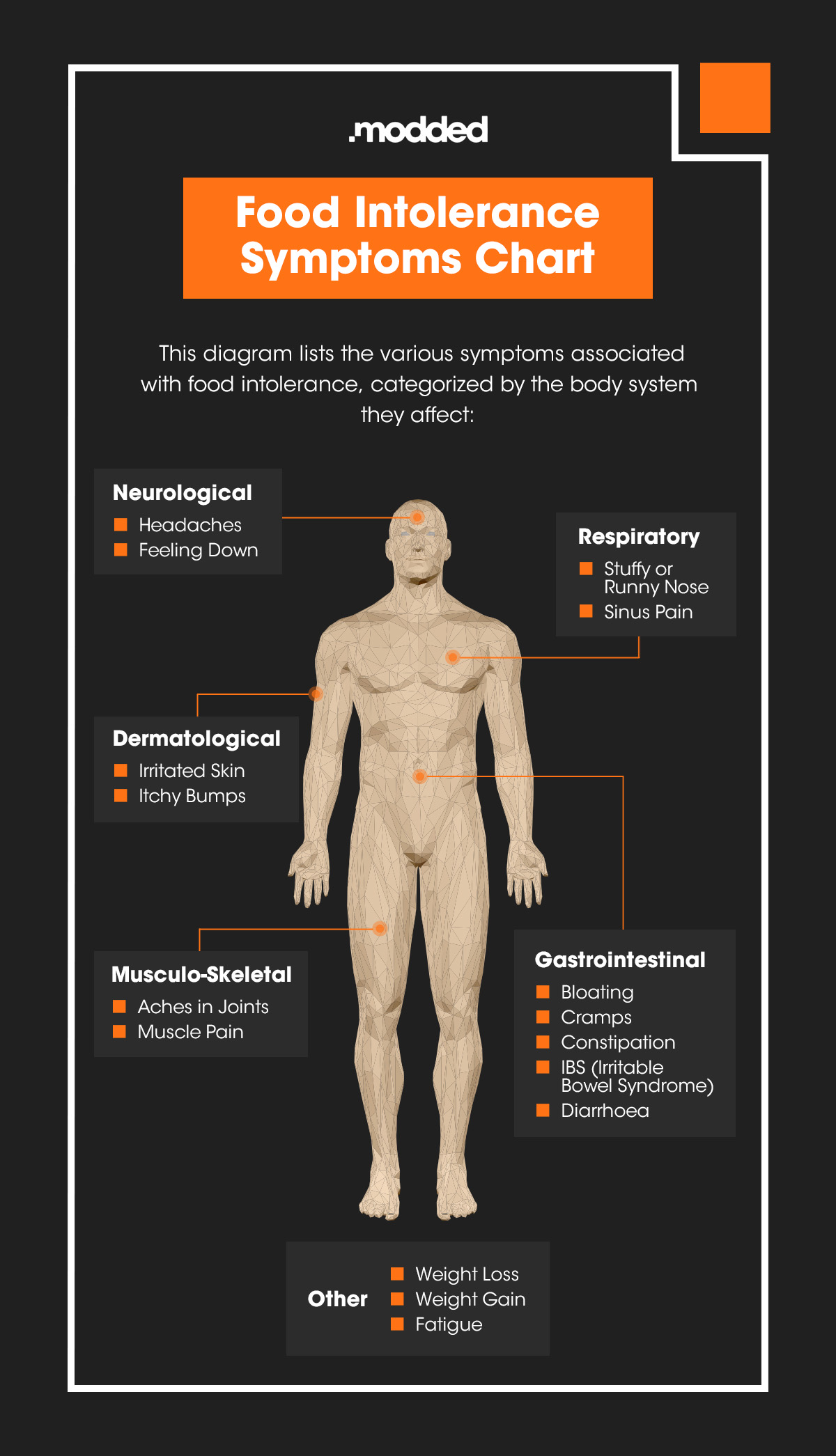
We fully break down the symptoms of food intolerance in the micrographic below:
Carbohydrate Intolerance Foods to Avoid — or Limit
Not all carbs are created equal. If you suspect carbohydrate intolerance, consider cutting back on:
- High-sugar foods: Soda, candy, pastries.
- Refined grains: White bread, pasta.
- Dairy if lactose is an issue.
- Some vegetables like onions, garlic and cauliflower.
- Legumes like beans and lentils.
Processed foods, especially those high in added sugars and artificial ingredients, can worsen symptoms. These foods cause rapid blood sugar spikes, leading to fatigue and cravings. Avoiding high-glycemic foods and opting for whole, minimally processed options can make digestion easier.
Alcohol, especially beer and sweet cocktails, can also contribute to symptoms due to their carbohydrate content and effect on gut health. Artificial sweeteners found in diet sodas and sugar-free products can also trigger digestive issues in some people.
The FODMAP diet can be used to determine which foods you need to avoid. You begin with a low-FODMAP meal plan for 6-8 weeks, then gradually reintroduce FODMAP foods for the next 6-8 weeks to figure out specific triggers.
What You Can Eat Instead
The good news? You don’t have to make carbs your mortal enemy. Instead, focus on low-glycemic, fiber-rich and easily digestible options like berries, citrus, quinoa, brown rice, oats, lean proteins, healthy fats and fermented foods for gut health.
Leafy greens, zucchini, bell peppers and cucumbers are great low-carb vegetable options that provide essential nutrients without causing digestive distress. Incorporating bone broth, collagen and anti-inflammatory herbs like ginger and turmeric can also help support digestion.
Resistant starches, such as those in green bananas, cooked and cooled potatoes and legumes, can also be beneficial. These carbs nourish healthy gut bacteria and help regulate blood sugar levels without causing drastic spikes.

How to Reverse Carbohydrate Intolerance
Managing carbohydrate intolerance doesn’t mean giving up delicious food — it just means being more mindful of what works for your body. Here’s how you can take control:
- Track your symptoms: Keep a food journal to help identify triggers and patterns in how your body reacts to different carbs. Consider monitoring not just what you eat but also your energy levels, mood and digestion.
- Modify your diet: Follow a low-carb or protein-based approach to reduce sensitivity to carbs. These diets keep you fuller longer, which helps regulate blood sugar and digestion Consider experimenting with portion control rather than eliminating all carbs at once. Gradually reducing carb intake can prevent withdrawal-like symptoms and cravings.
- Stay active: Regular exercise improves insulin sensitivity and blood sugar management. Strength training and low-impact activities like walking or yoga can be particularly beneficial. High-intensity workouts can boost glucose metabolism and overall energy levels. Before workouts, if you don’t have fructose intolerance, snack on high-carb fruits or take oatmeal and Greek yogurt to fuel the body throughout the workout. If you’re trying to bulk up, you need good carbs for energy and vitamins to help you maintain an active lifestyle.
- Practice stress management: Chronic stress can impair digestion and exacerbate symptoms. Techniques like meditation, deep breathing or even short breaks during the day can make a difference. Managing cortisol levels through better sleep and relaxation techniques can also improve insulin sensitivity.
- Hydrate: Because 60% of the body is water, drinking enough water and consuming electrolyte-rich foods can support digestion and reduce bloating. Men should consume about 3.7 liters per day. During workouts, consume 35 ounces every hour to maintain proper hydration levels. Dehydration can slow digestion and aggravate symptoms, so increase water intake to facilitate digestion.
- Improve gut health: Probiotics and prebiotics can help balance gut bacteria. Fermented foods like kimchi, sauerkraut and kefir promote a healthier gut microbiome. Reducing inflammation through a diet rich in omega-3s — found in salmon, walnuts and flaxseeds — can also improve digestion.
- Use enzyme supplements: Lactase or digestive enzyme supplements can aid digestion for certain foods, relieving bloating and discomfort. Alpha-galactosidase — found in supplements like Beano — can help break down certain carbohydrates in beans and cruciferous vegetables.
- Work with a nutritionist: If symptoms persist, consult a registered dietitian or nutritionist who can help tailor a personalized plan to manage your carbohydrate sensitivity. Customized meal plans, blood tests and microbiome analysis can provide deeper insights into food sensitivities and gut health.
Control the Future of Your Food Journey
Carbohydrate intolerance doesn’t mean a lifetime of restriction — it’s just a sign that your body thrives on a different balance of foods. Many men find that after identifying their triggers, they can effectively adjust their diet and make lifestyle changes to improve overall health and wellness.